Tissue engineering offers a solution for the treatment of disc herniations: an implant that combines synthetic hydrogel and living cartilage cells

Between the vertebrae of our spine are small but important bio-mechanical "pillows": the intervertebral discs, known to us mostly by the term "herniated disc". When these discs are damaged or degenerate, we suffer from back pain that can be extremely severe. These back pains cause suffering, impairment of function and economic damage to hundreds of millions of people in the world.
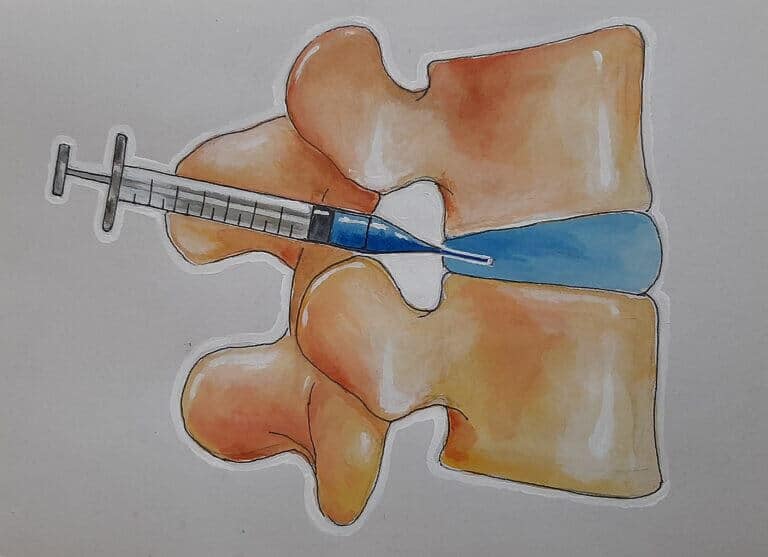
Today, these patients are offered conservative treatments, such as rest and physiotherapy, or surgeries, which in many cases are not helpful or even cause harm. Since the self-healing ability of the intervertebral discs is limited, there is a huge need for an implant that can take the place of the damaged natural disc, relieve the patients' pain and allow them to function as normally as possible.
The importance of the discs stems from the heavy burden, literally, that our spine carries. The spine supports the entire weight of the upper body, and is involved in a wide variety of movements and positions; The intervertebral discs are responsible for transferring and distributing the loads involved in these movements. To create an artificial implant that will meet these challenging tasks, the structure and function of the natural disc must be imitated. Prof. Sharit Sion and Dr. Michal Amit from the Baruda Academic College of Engineering in Karmiel accept the challenge and mobilize tissue engineering methods for this purpose.
Life in a box
To create an implant that best combines the mechanical strength and the disc environment suitable for cell growth, the researchers use the hydrogel developed by Prof. Sion during her postdoctoral work at the University of Oxford in England. The hydrogel mimics the biomechanical and physical properties of the intervertebral discs (strength, flexibility and salt concentration), and is intended to serve as a suitable three-dimensional environment for the cells that will live and function within it.
The researchers hypothesize that the special structure of the implant will allow the cells to function in a way similar to the one in which they function in the natural intervertebral disc: to thrive and create a characteristic intercellular texture, and to prevent the growth of nerve cells in the place vacated by the degenerated disc. The growth of nerve cells in the space between the vertebrae is probably responsible for the typical back pain in the case of a damaged or degenerated disc.
The current challenge faced by the research group, which also includes research assistant Dr. Iris Bonstein, is to allow the cells to thrive within the hydrogel - which, although endowed with desirable biomechanical properties, is also very acidic, and therefore may be a challenging environment for the cells. The researchers therefore chose stem cells that had undergone differentiation into cartilage cells, and examined two main ways of inserting them into the hydrogel. One is the seeding of exposed cells directly inside the hydrogel and the other is inserting them into the hydrogel when they are packed inside a cover (capsule).
Sowing in clusters
The packaging of the cells in the capsules was found to be inappropriate, as it damaged the biomechanical properties of the implant. Seeding of single exposed cells did not fare well either, because they did not survive in the acidic environment of the hydrogel. Instead, a third way was found: to sow the cells without an envelope, but not individually either, but in clusters of many cells adjacent to each other. Thus, even if the outer cells in the cluster died, the inner cells remained alive and even functioned well: they secreted proteins, which are necessary to create the extracellular environment characteristic of the disc. It is hoped that over time, the cells that multiply will gradually replace the hydrogel, and the biological component will be an increasing component of the implant.
In addition to this, in a study that won a grant from the National Science Foundation, it was found that endothelial and nerve cells do not multiply in and on top of the gel, and do not build neural networks and blood capillaries in a culture grown on or within a hydrogel. Since the growth of nerve cells to the place vacated by the degenerated disc is what probably causes back pain - this is a very encouraging finding.
The studied hydrogel is therefore suitable for growing cartilage cells, which survive and enrich their environment with proteins. Thanks to the physical properties of the hydrogel and the living cells in it, the implant may well replace a degenerated or damaged disc.
In the next phase of their research, the researchers will continue to examine the function of the implant in a living body, and will even try to integrate it into an external shell that simulates the outer part of the disc. In this way, one active unit will be created, imitating the physiological activity of the entire disc. This step in the research may bring about a revolution in the healing methods of the spine, ease the suffering of many patients and save many resources devoted to their treatment.
From a wider research and medical point of view, this type of implant will be a leap forward in tissue engineering at the level of the whole organ, which will be possible to apply in the development of additional and diverse types of implants.
Life itself:
Prof. Sharit Sion and Dr. Michal Amit share a common love for plants and gardening. Prof. Sion enjoys designing spaces and gardens, and Dr. Amit grows and multiplies orchids in her office.
