Perceptions of aging by elderly patients affect their health after hospitalization
Do "perceptions about aging" at an early point in time predict the physical functioning of elders facing health challenges after hospitalization? This is the subject of Dr. Jacob Hoffman's research, in collaboration with Prof. Amit Shira and Prof. Ehud Bodner from the Gerontology Program at Bar-Ilan University. The research, which won a grant from the National Science Foundation, will examine approximately 500 patients from several internal departments in three hospitals, who will be evaluated at four time points during six months of their hospitalization.
The relationship between perceptions of aging and coping with health challenges was demonstrated in a preliminary study in 226 elderly people suffering from various chronic medical conditions, such as stroke or osteoporotic fractures (with hospitalizations). A younger subjective age (people who felt younger than their age) at the time the patients were admitted to the hospital, predicted higher assessments in the functional independence measurement upon discharge. The functional independence index is an evaluation tool whose purpose is to assess the functional status of patients throughout the rehabilitation process following a stroke, traumatic brain injury, spinal cord injury or cancer. These findings show that several key perceptions about aging predict health outcomes among older patients hospitalized or in the community with serious medical conditions.
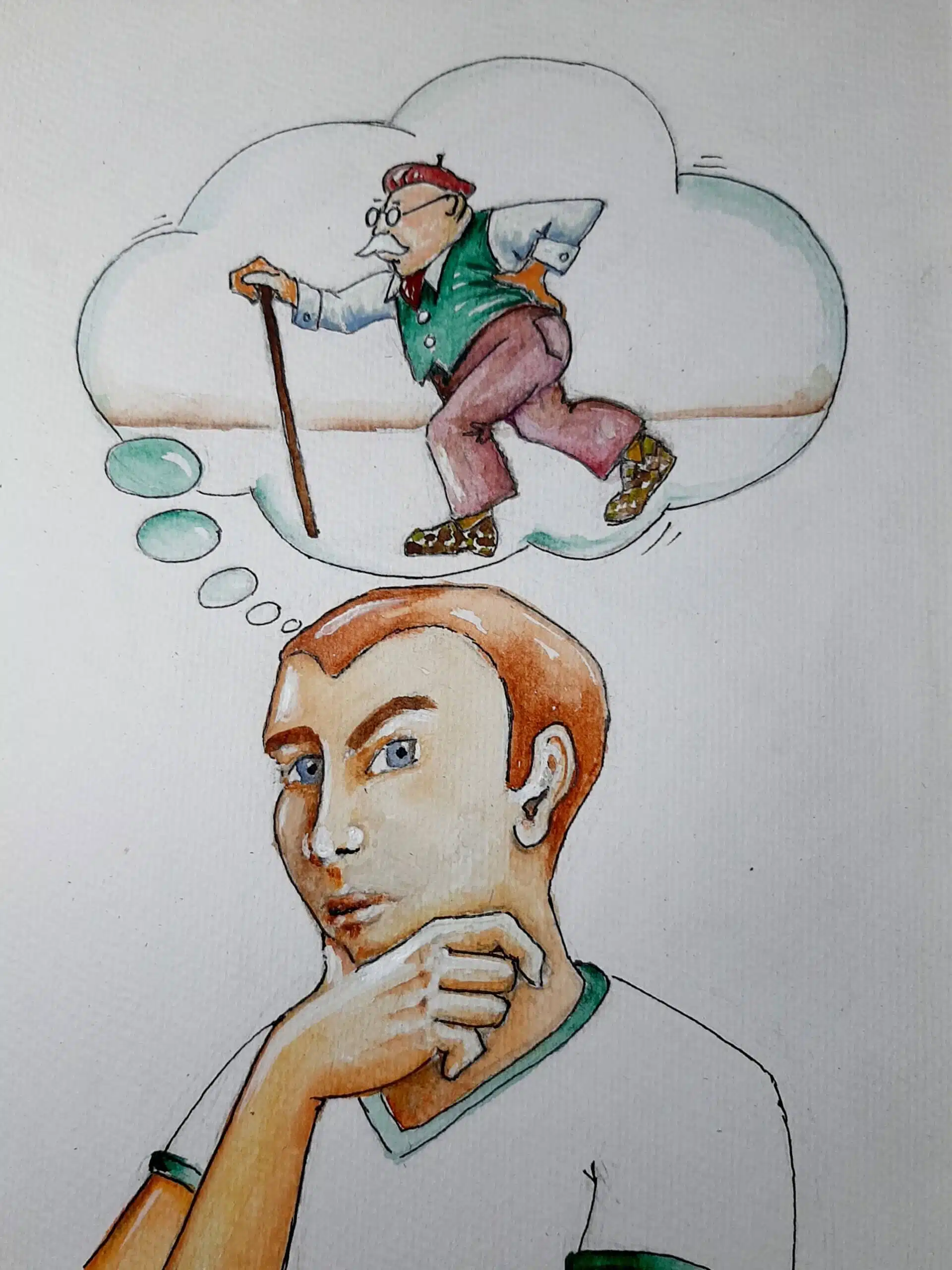
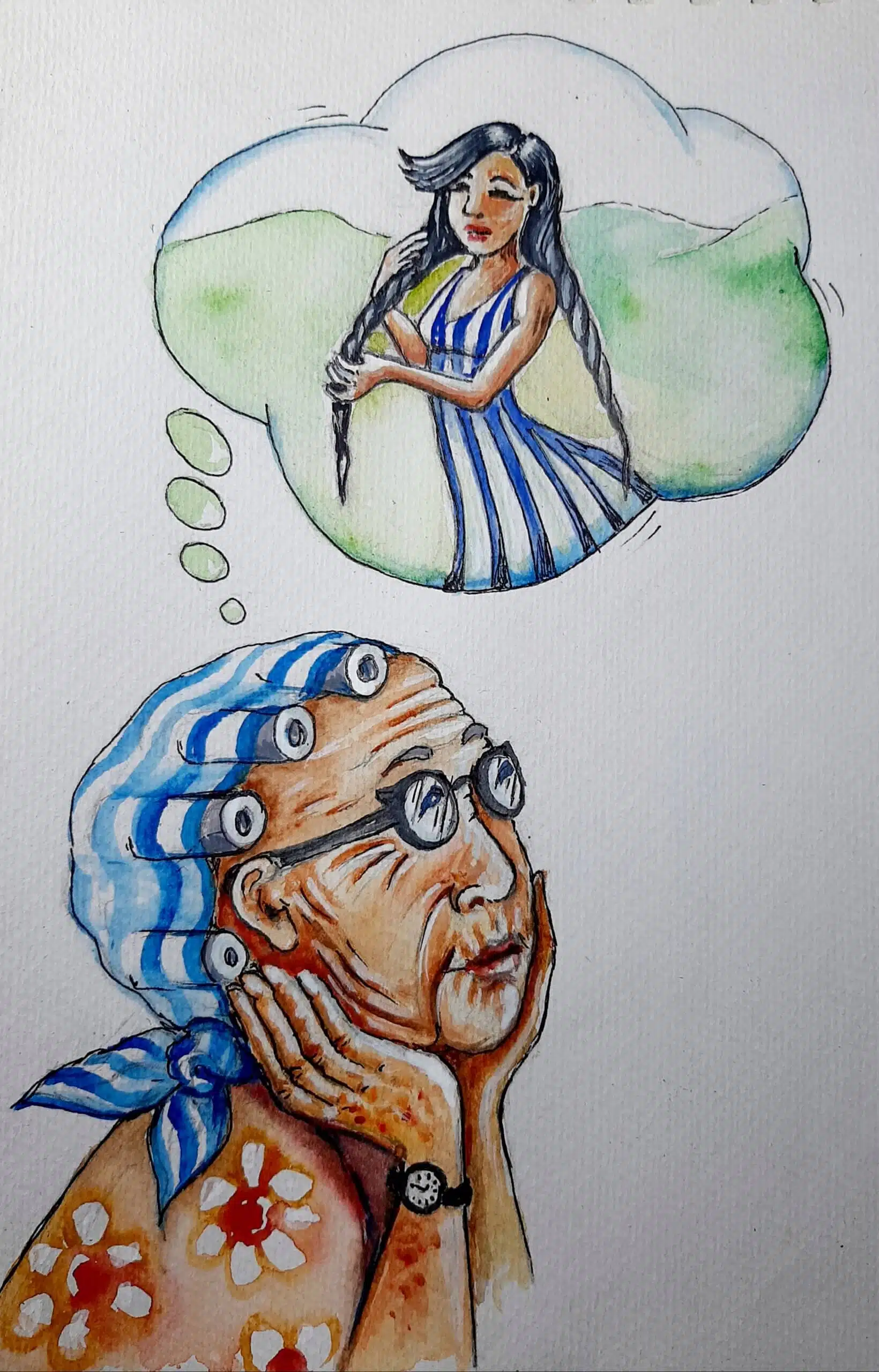
The elderly population is hospitalized more than other age groups, especially in internal medicine departments, where the elderly make up 65-70% of those hospitalized. Hospitalizations are an important crossroads in the lives of older people that can have a dramatic effect, and ultimately lead to deterioration or recovery. Based on the scientific literature, 'perceptions about aging' (eg ageism) can largely predict the health and functioning of the older person. The early findings of the researchers, which were supported by previous evidence, show that 'perceptions of aging' measures can predict health and physical functioning even among elderly people suffering from a chronic disease, as well as among elderly people hospitalized in a rehabilitation unit. The present study aims to test an integrative model that links several main 'perceptions of aging': negative stereotypes about old people (ageism), perceptions of self-aging (attitudes towards self-aging and subjective age) and awareness of age-related change. The study therefore suggests that these 'perceptions of aging' will work together and affect health and physical function after hospitalization.
In addition to direct effects, for example, ageism affecting health and physical functioning, the researchers predict that the level of ageism at the beginning of hospitalization will affect perceptions of self-aging (i.e. negative attitudes towards aging or older subjective age) later in hospitalization, which in turn will lead to awareness of age-related change (in the sense the negative) after discharge, which will eventually lead, six months later, to poor physical health and functioning. The scientists believe that the relationship between ageism and perceptions of self-aging will be dictated by the level of ageism of the medical staff, that is, the higher the departmental ageism (in the hospital where they were admitted), the stronger the relationship between the patients' ageism and their perceptions of self-aging.
Dr. Hoffman says the research may have theoretical as well as practical implications. Theoretically, this study advances the field of 'perceptions of aging' by referring to the unique connections between several 'perceptions of aging' and their impact on health, in the common context of hospitalization. Practically, the findings may guide different types of interventions that will target specific perceptions of aging among patients, with the aim of improving their health after hospitalization. Finally, understanding how ageism in the medical department may affect patient health outcomes will lead to macro-level interventions, such as appropriate training of medical professionals.
Life itself:
Dr. Hoffman likes to travel with his family, read books, swim and study the daily newspaper. He has a dream, to buy a surfboard and go to the beach once a week. Sometimes, as we know, dreams come true.
More of the topic in Hayadan:
