Weizmann Institute of Science scientists have developed a new approach to immunotherapy based on communication between the cells of the immune system
To achieve results on the battlefield requires a combination of forces of accurate intelligence and determined warriors. However, in the environment of the cancerous tumor, the fighters of the immune system - T cells - very quickly lose their killing ability and become exhausted, while the intelligence envelope of the dendritic cells is scarce. This is one of the reasons why the great promise of immunotherapy - the new generation of treatments harnessing the immune system to fight cancer - is not fully realized. In a new study, Published today in the scientific journal Cell, Weizmann Institute of Science scientists present an antibody they developed that connects T cells and dendritic cells to create a powerful immune response against cancer. The research opens a window to a new approach in immunotherapy: the development of treatments that connect different cells of the immune system to assemble an effective battle team against cancer and other diseases.
One of the immunotherapy treatments that lead the revolution in biological cancer treatment in the last decade uses antibodies that block PD-1 - a checkpoint receptor found on the surface of T cells. When this receptor is expressed on T cells, a protein in the tumor environment may bind to it and transfer the cells T to the state known as "exhaustion". PD-1 antibodies prevent the protein from binding to T cells and suppressing it, but a large number of patients do not respond to this treatment at all - and in many others its effectiveness is limited in time.
In order to develop a more effective immunotherapy, scientists from the laboratories of Dr Roni Dahan and Prof. Ido colleague In the department of systemic immunology at the institute, where the existing treatment failed. To do this, they sampled T cells from a mouse model of two types of cancer treated with PD-1 antibodies. "Using advanced technologies of RNA sequencing at the single cell level and big data algorithms, we examined almost 130 thousand T cells, some of which responded to treatment and some of which did not," explains Prof. Amit. "Surprisingly, the group of T cells that did respond to treatment expressed genes that indicate an interaction with a rare population of dendritic cells."
Dendritic cells are professional antigen presenters, which means they collect intelligence throughout the body by ingesting molecules belonging to disease-causing agents, and present the findings to T cells in order to alert them to a foreign invader or cancerous transformation, and motivate them to action. The anti-PD-1 treatment in itself is supposed to help activate T cells that fight cancerous tumors, but when they looked at a mouse cancer model without dendritic cells, the researchers saw that the treatment completely lost its effectiveness. In other words, they recognized that the dendritic cells are essential for the proliferation and activation of specific T cells against the cancer, and therefore necessary for the success of the entire treatment.
These discoveries revealed a major weakness of the existing treatments, as the population of dendritic cells is quite rare in many of the tumors and in the majority of patients currently receiving anti-PD-1 treatment. In this situation, there is a low probability of an encounter between these cells and the T cells they activate. This understanding paved the way for the engineering of a new antibody called BiCE (short for Bispecific DC-T Cell Engager) whose two arms were designed to connect two different cells - one binds a T cell and blocks the PD-1 receptor, similar to existing treatments, while the other recruits a dendritic cell from the population the rarity that is essential for the activation of T cells. Those who led the research of the new treatment are doctoral research students Yuval Shapir Itai from Dr. Dahan's laboratory, and Oren Barboy, from Prof. Amit's laboratory.
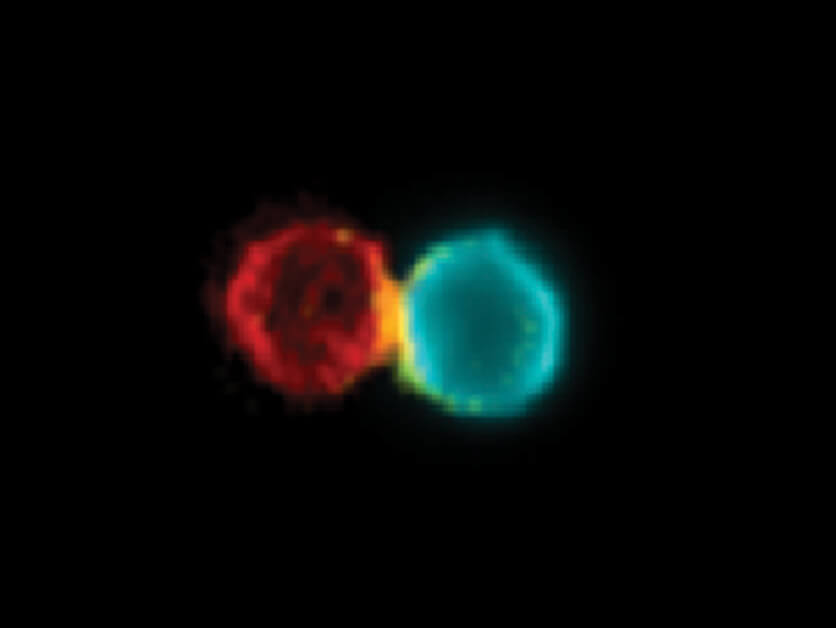
After developing the antibody, the scientists tested how it works. When we fluorescently labeled the antibody and the immune cells of mice with skin cancer that received the new treatment, the resulting image clearly showed how the antibody physically connects a T cell to a dendritic cell and increases the amount of pairs of these cells in the tumor environment and in the lymph nodes adjacent to it. It was also discovered that the pairs formed by the antibody were active and created an immune response against the tumor. Furthermore, following the treatment, dendritic cells that were in the vicinity of the cancerous tumor, migrated to the lymph nodes and joined the T cells located there in order to share the intelligence information with them and activate them.
Hope for the treatment of incurable diseases
The effectiveness of the new treatment was tested in a study on several murine models including aggressive breast, lung and skin cancer. The growth rate of skin and lung cancers decreased significantly with the treatment with the new antibody, compared to the existing treatment. On the other hand, breast cancer that does not respond to the existing treatment also did not respond to the new antibody. The researchers hypothesized that the reason for this is the very low number of active dendritic cells in the environment of this tumor. Therefore, they tried a combined treatment with the newly developed antibody, along with a known treatment that increases the level of activity of dendritic cells in the tumor environment. The combined treatment was found to be the most effective of the existing options and showed that even in cancers that have not yet responded to immunotherapy, synergy between T cells and between active dendritic cells creates a strong immune response against the tumor.
In the next step, the scientists checked whether, along with a strong immune response, the new antibody succeeds in preventing the disease from returning in the future. In many cancer patients there is a recurrence of the disease, even after the central tumor has been removed and the known metastases have been treated. The most significant risk that worries most patients is tiny metastases that slip under the radar and develop over time into renewed cancer. BiCE, unlike the existing treatment, was found in a study to be effective also against the development of lung metastases after the removal of the central tumor. The researchers hypothesize that this is evidence that the antibody manages to produce a systemic immune response throughout the body against the cancer, and even leave after the treatment immune cells that remember how to recognize the cancer and react against it.
Company “ידעThe person responsible for the commercialization of the intellectual property of the scientists of the Weizmann Institute of Science, recently submitted an application for the registration of a patent for these findings, with the aim of developing an innovative treatment based on the antibody developed by the scientists of the institute. "We present here a new approach that emphasizes a systemic view of immunotherapy," says Dr. Dahan. "Instead of concentrating on one pathway, we engineer antibodies that serve as a platform for communication between different immune cells of our choice. This is a development that gives hope not only to cancer patients, who require activation of the immune system against the tumor, but also to patients with various diseases, such as autoimmune diseases, where the patients need immune suppression of the reaction against the body itself. Comprehensive methods for suppressing the immune system exist, but I believe that our innovative approach will make it possible to suppress and activate targeted immune responses, without the wide and dangerous consequences of general suppression and activation of the immune system."
Dr. Ran Salomon, Dr. Ken Shay and Dr. Eitan Winter from the Department of Systemic Immunology at the Institute also participated in the study; Achaied Berkowitz and Prof. Amos Tani from the Department of Computer Science and Applied Mathematics at the Institute; Tamar Shami and Prof. Neta Erez from the Tel Aviv University School of Medicine; and Dr. Ziv Porat from the Department of Life Science Research Infrastructures at the Institute.
More of the topic in Hayadan:
- The balance between the populations of dendritic cells in the intestine is a condition for the proper functioning of the digestive system
- The club - what do cells of the immune system do in selected meeting places in the bone marrow?
- Caution, metabolic syndrome
- The flexible genetics of gut bacteria
- A fish explores a fish
