35% of the corona patients who died in the epidemic were diabetics. In a new study, Weizmann Institute of Science scientists reveal that high blood sugar levels disrupt the immune system's ability to fight lung infections and present a therapeutic approach that may save lives
In 2020, with the outbreak of the Corona epidemic, a scientific question that remained unanswered was revisited in full force: Why were 35% of patients who died from complications of Corona also diabetics? Years before, it was already known that diabetics are at increased risk of complications due to exposure to respiratory pathogens, but the reason for this sensitivity remains a mystery. In a new study Published this week in the scientific journal Nature, Weizmann Institute of Science scientists reveal that high blood sugar levels damage the function of a subset of the immune system cells in the lungs and thus disrupt the immune response against respiratory infections. The scientists from the laboratory of Prof. Eran Alinev In the Department of Systemic Immunology, therapeutic approaches are presented in research that may make it possible to significantly reduce the risk posed to diabetic patients from respiratory tract infections.
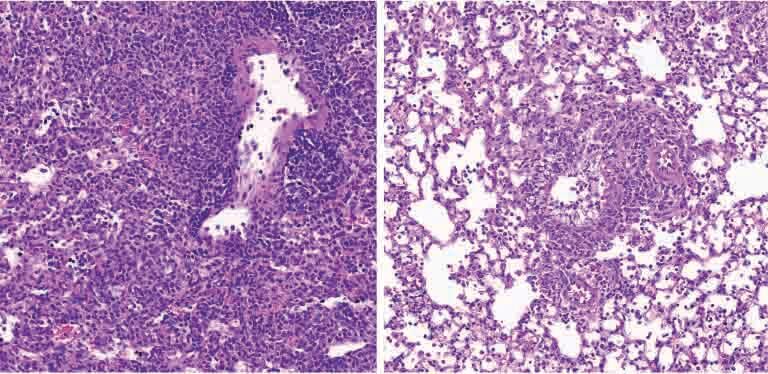
More than 500 million people worldwide are dealing with diabetes, and the prevalence of the disease is expected to increase even more in the coming decades. Since both diabetes and respiratory diseases are two of the most common causes of death in the world today - 9th and 4th respectively - understanding the relationship between them is expected to have far-reaching medical consequences. To shed light on this connection, the research team in Prof. Alinev's laboratory, led by Dr. Samuel Noves, Dr. Alexandra Kolodzica and Dr. Sahib Abedin, examined what happens in a mouse model of type 1 and 2 diabetes when exposed to various viruses of ways of breathing. Similar to diabetic humans, when the diabetic mice were exposed to pulmonary pathogens, such as the influenza virus, they developed an acute and even fatal lung infection. In an attempt to find the cause of this sensitivity, the researchers analyzed the differences in gene expression in more than 150,000 lung cells of diabetic and non-diabetic mice using advanced methods for sequencing the genetic material at the single cell level. In addition, the researchers analyzed in depth the gene expression in the immune system cells in the lungs of the infected diabetic mice.
The series of tests revealed a malfunction of the cells of the immune system called dendritic cells - cells whose role is forever to implement a targeted and effective immune response against pulmonary infections. "High blood sugar levels severely disrupt the activity of a subset of dendritic cells in the lungs, impairing the ability of these gatekeepers to send the molecular messages required for the activation of an effective immune response," says Dr. Nobbs. "As a result, the infection in the diabetic mice spread unchecked."

But what is the mechanism by which high blood sugar levels disrupt the normal function of pulmonary dendritic cells? The researchers identified that high blood sugar levels led to changes in the metabolism in these cells and the accumulation of metabolic byproducts which in turn disrupted the genetic control mechanisms of the cells and damaged the production of the proteins needed for an effective immune response. "The mechanism we found can explain why the immune system of diabetics is unable to fight effectively against pulmonary infections," says Dr. Kolodzica.
""These findings are particularly exciting, as they mark a therapeutic horizon and show that it is possible to overcome the tendency of diabetic patients to develop acute lung infections"
After uncovering a mechanism that disrupts the functioning of the immune system in diabetes, the scientists examined whether and how this failure could be prevented. The scientists showed that tight control of blood sugar levels in the diabetic mice through the administration of insulin improved the dendritic cells' ability to mount an effective immune response. Alternatively, giving small molecules capable of preventing the molecular disruptions caused to the dendritic cells, allowed them to carry out an effective immune response - even when blood sugar levels remained high. "These findings are particularly exciting, as they mark a therapeutic horizon and show that it is possible to overcome the tendency of diabetics to develop acute lung infections," says Dr. Abedin and adds that the findings emphasize the need for careful monitoring of sugar levels in diabetics, including during illness.
"Our findings provide, for the first time, an explanation for why diabetics are more sensitive to respiratory infections," Prof. Alinev concludes. "Being more careful about blood sugar levels may reduce this distinct risk. However, there are diabetics whose sugar levels are more difficult to control, for whom the solution may be the development of drugs based on the small molecules tested in the study. It is possible that local inhalation treatment with these future drugs could increase their effectiveness and reduce their possible side effects."
Dr. Nir Khoresh, Dr. Gayatri Mohapatra, Dr. Ryan-James Hodgetts, Dr. Igor Spivak, Dr. Labial Flohar, Dr. Denis Koiatkowski, Dr. Meli Dori participated in the study. Bakhsh, Dr. Yiming Ha, Dr. Hagit Shapira, Christine Butchernikov, Ella Herzog, Sophia Heindorf and Sara Perini from the Department of Systemic Immunology at the Weizmann Institute; Prof. Ayelet Erez and Little Adler from the Department of Molecular Cell Biology at the Weizmann Institute; Prof. Alon Hermlin and Dr. Noa Stettner from the Department of Veterinary Resources at the Weizmann Institute; Dr. Alexander Brandis and Tebi Melman from the Department of Life Sciences Research Infrastructures at the Weizmann Institute; Dr. Jens Puschhof and Lena Schur from the German Cancer Research Center (DKFZ), Heidelberg, Germany; Dr. Aryeh Musayouf and Dr. Anish Zakaria from the Hebrew University in Jerusalem; and Prof. Manfred Kopf of ETH, Zurich, Switzerland.
More of the topic in Hayadan:
