A research group at the Faculty of Medicine at the Technion analyzed the aforementioned phenomenon and demonstrated methods of intervention that may curb it
A study conducted at the Rappaport Faculty of Medicine at the Technion sheds light on the mechanisms that lead to the fact that even successful chemotherapy may lead to the development of cancer metastases - the main cause of death from cancer. The article, which was published a few days ago in the journal Cancer Research, was chosen to be published on the cover of the issue and was also awarded an opinion article by the editors of the journal at the beginning of the issue.
Prof. Yuval Shaked and PhD student Josephina Haj Shumeli, who led the research, explain that the existing practices for the treatment of cancer demonstrate great effectiveness and in many cases save lives, as demonstrated both in clinical studies and in the data accumulated over the years. However, they say, there are patients who do not respond to treatment, and sometimes the disease erupts after treatment more aggressively, including metastases in other organs such as the lungs. The article explains the mechanism that causes the outbreak of metastases after treatment even in cases where the treatment successfully damages the primary tumor.
The researchers focused on the development of Lung tissue metastases Following Chemotherapy for breast cancer. Breast cancer is the most common malignant tumor among women and occurs, at a low rate, in men as well. The survival rates of these patients in Israel are increasing thanks to the early detection of the disease and the improvement of treatment technologies. However, when the tumor metastasizes to other organs, the chances of recovery plummet. According to statistics, approximately 30% of patients diagnosed with early-stage breast cancer, and treated with conventional means, are expected to develop metastases within a few months or a few years.
Metastases originating from breast cancer are partly due to the proximity of the breast to the lymph nodes in the armpits. This proximity makes it easier for cancer cells to reach the lymphatic system from the breast, which is a branched system of tubes much like the blood system. Through the lymph fluid the cancer cells migrate to other organs such as lungs, liver and bones, where they metastasize.
The question that preoccupies many cancer researchers, against this background, is which conditions help the metastatic process and which medical interventions may inhibit it. According to Prof. Shaked, "Today it is known that the metastatic process is not completely random. The metastases thrive in tissues where they find mechanical support and a supportive cell environment."
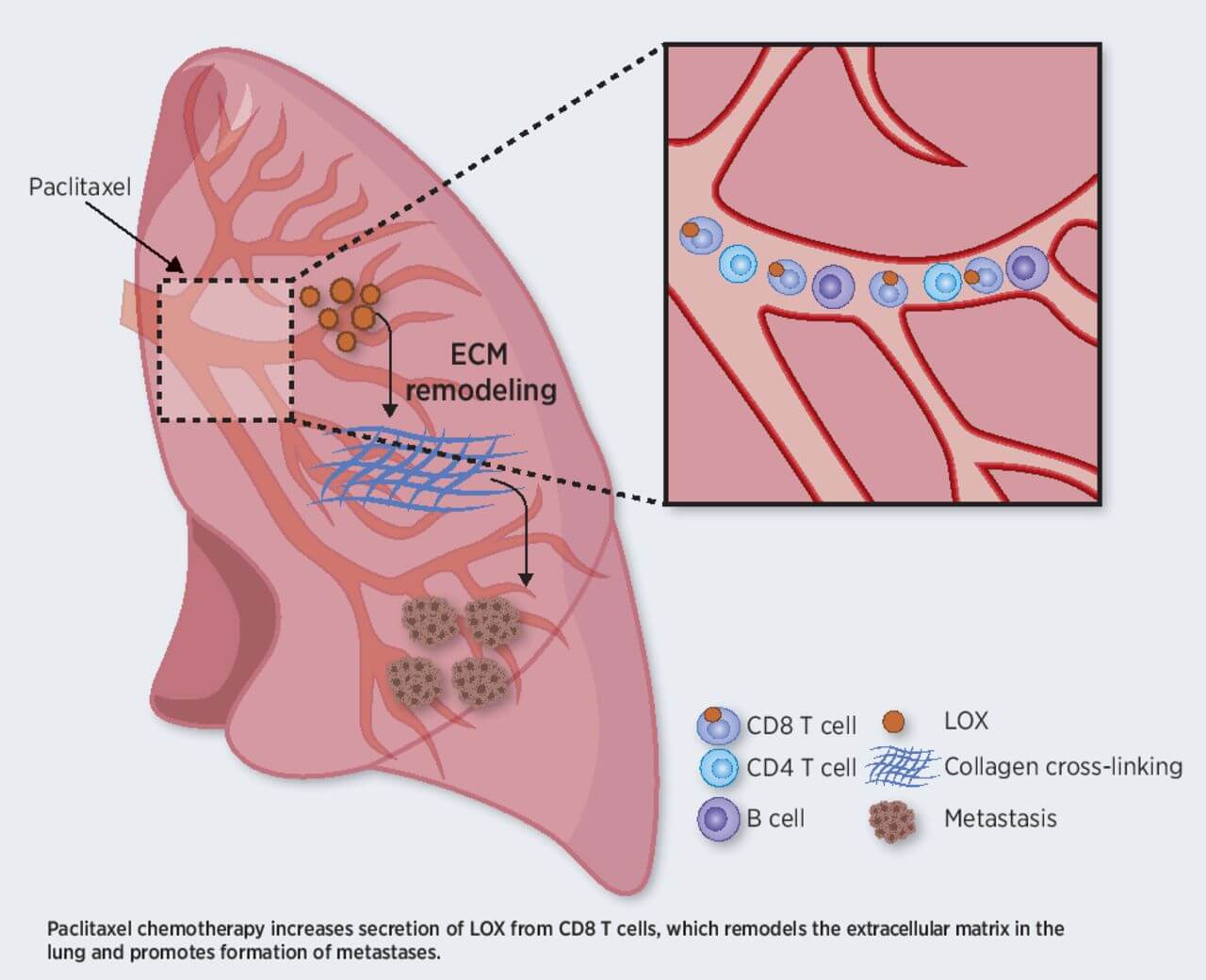
Prof. Shaked's research group discovered in previous studies that a common enzyme called LOX, which affects the configuration of the tissue, may change the lung tissue in a way that makes it easier for cancer cells to stick to it and develop metastases in it. When the researchers inhibited the activity of that enzyme, a significant reduction was achieved in the ability of the cancer cells to adhere to the lung tissue and thus the formation of cancer metastases was reduced.
Also in the current study, the researchers focused on the LOX enzyme, but this time in a different context - his involvement בDevelopment of metastases following its secretion from specific immune cells: CD8 type T cells+.
LOX enzyme is found in a high dose in the lung tissues even in the healthy person, but this dose increases rapidly and dramatically in response to the chemotherapy treatment. Contrary to popular belief, according to which this enzyme is expressed in mesenchymal cells, the Technion researchers discovered to their surprise that the increased dose of LOX is actually due to its increased secretion by the cells of the immune system - those CD8 type T cells+. The increase in the presence of this enzyme affects the properties of the lung tissue and makes it the favorable environment for cancer cells. This phenomenon can explain why some patients undergoing chemotherapy develop metastases even after successful initial treatment. The explanation, as mentioned, is in the effect of the chemotherapy on the lung tissue in such a way that this tissue becomes comfortable for cancer cells.
"When we talk about the lung environment in this study," explains Prof. Shaked, "we are referring to the ECM, the extracellular environment in which the cells reside. It is a complex network of proteins that supports the cell structurally and mechanically as well as in terms of various functional aspects. In the present study we discovered that the activity of LOX harnesses the extracellular environment in favor of the cancer cells. Following the changes that the T cells and the LOX enzyme generate in this medium, it begins to help the cancer cells grow, survive, move, divide and adhere to each other. Moreover, he may block entry of normal immune cells and even of anti-cancer drugs to the malignant region."
The study was conducted in a model of breast cancer in mice and the anti-cancer drug paclitaxel, but the researchers estimate that its findings are also relevant to other drugs and other types of cancer, which is expected to be tested in future clinical studies. According to PhD student Josephina Haj Shomeli, "We were surprised to find that the mechanisms of action we uncovered, which encourage the development of cancer metastases, are activated not only in response to surgery as found in the past, but also in response to chemotherapy and possibly additional drugs that we are currently investigating."
"Our achievement - locating the mechanism that causes the structural change in the lung by the immune system - may make it possible to develop drugs and combined treatments that will prevent this phenomenon and reduce the chances of developing metastases," says Prof. Shaked. "We are now working on developing barriers to the various proteins that cause the same structural change in the lung tissue. We believe that the research findings will lead to an updated definition of the bank of therapeutic targets and the use of LOX inhibitors to curb metastatic developments."
The research was supported by BSF (Binational US-Israel Science Foundation), ERC (European Research Commission) and ISF (Israel National Science Foundation). Doctoral student Josephine Haj is a scholar in the Ariane de Rothschild program for female doctoral students - a program that promotes outstanding doctoral students in order to integrate them into key positions in Israeli academia and society.
לThe scientific article in the journal Cancer Research
More of the topic in Hayadan:
- Changes in the lung tissue indicate preparation for the absorption of breast cancer cells
- Researchers at Tel Aviv University revealed the mechanism responsible for introducing copper ions into the cell
- Chemotherapy for lung cancer is now available in capsules for swallowing
- Groundbreaking research: a new protein has been found that significantly inhibits cancer metastasis
