Technion researchers have developed a smart plaster that closes the surgical incision by itself and also accelerates and monitors the healing process
Imagine surgery without stitches, without staples and without glue, using a smart plaster that not only closes the surgical incision but also monitors its condition and accelerates its healing. What's more, this patch is attached to the skin לפני The operation is the one that helps to pin the two sides of the incision together.
Strange, almost imaginary, but the aforementioned concept was developed into an active prototype whose effectiveness was demonstrated in a study published in the journal Advanced materials. The unique plaster, which provides ongoing information on the condition of the tissue during and after the operation, was developed by Prof. Hussam Haik and post-doctoral student (now Prof.) Ning Tang from the Wolfson Faculty of Chemical Engineering.
Surgery with the conventional method is based on cutting the tissue, performing the necessary operations and reclosing the injured tissue. This closure is done in invasive ways such as sewing and joining with staples, which also damage the healthy tissue around the tear and in many cases create new complications. The monitoring of tissue restoration is also very limited, since if the surgery is on an internal organ it is difficult to monitor it, and even if it is not internal, any condition assessment requires removal of the dressing, which opens up the possibility of contamination of the site. Finally, the assessment of the state of the tissue in the various stages after the operation is done visually - the doctor's view - which of course has a subjective element and cannot accurately assess the rate of healing or detect inflammation that is not visible to the eye.
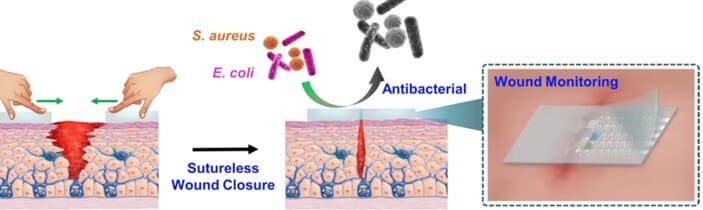
"The technology we have developed will in many cases eliminate the need for staples, stitches and normal dressings," explains Prof. Haik. "The smart patch includes a polymer substrate that includes an array of sensitive sensors for monitoring chemical and physical indicators in the wound environment. Both the polymer substrate and the sensors have the ability to self-reconnect after tearing or cutting. The smart patch is glued to the tissue before cutting and the tissue is cut through it. Since the patch is characterized by self-healing capabilities, without the need for external technical aids, pulling the two sides of the cut patch together returns it to its initial state within a few seconds. While fusing, the plaster pulls the tissue it is glued to until it is completely closed. The patch continues to hold the two parts of the cut in the tissue autonomously until the process of biological fusion of the cut is complete."
During all stages of the surgery and healing, the sensors of the smart plaster continuously monitor essential physiological indicators including temperature, PH and glucose levels in the connective tissue. These indicators provide an indication of the state of healing of the connective tissue, the potential involvement of infections, the development of physiological disorders, etc. According to Prof. Haik, "In contrast to the visual assessment used today, the smart patch will provide the doctor with a kind of 'chemical eyes' to monitor the tissue without the need to remove the dressing."
The various physiological data is transmitted by the patch through a smartphone to the treating team, who receives a detailed and objective picture of the situation without having to expose the incision. What's more, the plaster releases antibacterial substances that speed up the recovery.
The idea of an artificial electronic sheet that heals itself was demonstrated in previous studies in Prof. Haik's laboratories, which demonstrated impressive success in the development of such sheets and in applications related to the fields of robotics and the fourth industrial revolution. However, in the new study, the researchers were required to develop new functional materials for assembling the sheet because here an adaptation is required for continuous attachment to biological tissue. In experiments on tissues in the laboratory and on animals, the researchers showed that the system succeeds in healing the cut tissue with an efficiency similar to that which is attached with the help of sutures or biological adhesives, but unlike the traditional way, it does so without using external aids and without leaving marks after the operation, as happens in healing with sutures. The animal experiments showed that the system does indeed provide a continuous and accurate update regarding the biochemical markers of the tissue during the healing process and accelerates the recovery. According to Prof. Haik, "the new technology expresses a new approach to performing and healing incisions during surgery and enables monitoring during recovery - something that is of crucial importance considering that wounds in the healing process, and even closed wounds, are exposed to pathogens such as bacteria, and therefore they also need to be carefully guarded and monitored at an early stage for inflammation and infections. In addition, the new technology can help heal various wounds and cuts and chronic wounds that do not heal by themselves."
Prof. Hossam Haik He is the head of the laboratories for advanced nanomaterials and dean of certification studies at the Technion. He leads research in a variety of fields that combine nanoelectronics, smart sensing and more for the benefit of medical applications, some of which are adapted to the needs of the third world.
Dr. Ning Tang He completed all of his degrees at Tianjin University and came to Haik's lab as a postdoctoral fellow. At the end of the post-doctorate, in the framework of which he conducted the current research, he was appointed an associate professor at Shahmai Jiao Tong University.
for the article in the journal Advanced materials
More of the topic in Hayadan:
- Hussam Haik presents: a new technology for the early diagnosis of stomach cancer
- Success in creating an engineered implant that replaces damaged bone tissue
- The nanotechnological artificial nose of Prof. Hussam Haik is applied in a patch for diagnosing tuberculosis
- Prof. Hussam Haik will receive a grant from the Gates Foundation to develop an autonomous system for diagnosing tuberculosis
- The smart electronic skin

2 תגובות
So when (and where) can we buy this patch for home use?
It must also smell.