Degeneration of the cells of the immune system in the brain may be the biological cause of depression, and there may be substances that can restore these cells - and be antidepressants
Depression is one of the main causes of human suffering and dysfunction and leads to most suicides. Its symptoms include low mood, loss of pleasure and interest (eg in social activities), feelings of worthlessness, guilt and regret, helplessness, despair and self-loathing, fatigue and apathy.
In the psycho-neuro-immunology laboratory at the Hebrew University, directed by neuroscientist Prof. Raz Yeremia, they are trying to discover new biological mechanisms of depression in order to develop new and more effective drugs based on them. Prof. Jeremiah: "The primary biological cause of depression is still unknown, therefore the existing drugs do not help many patients, or they take a long time to have an effect. One of the reasons for this is that most of the research on the disease focuses on functional problems of nerve cells (neurons) and does not examine the involvement of additional cells. We and other researchers changed direction and discovered that depression can be caused by disturbances in the immune system, and especially in its representatives in the brain - the microglial cells."
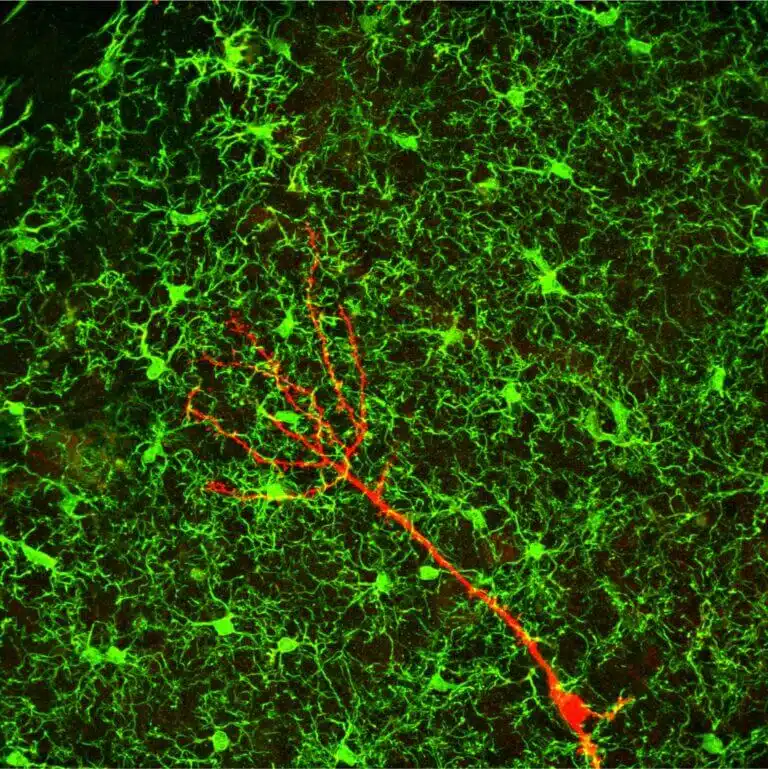
Microglia are cells of the immune system that enter the brain during the embryonic period, remain there to protect it from pathogens such as viruses and bacteria and from neurological diseases. In addition, they have many physiological roles in the brain, for example the creation and direction of connections between neurons in the development of the brain and the creation of new neurons (neurogenesis) in the hippocampus (a brain area that is essential for emotional and cognitive processing), and their connection to the neural network, i.e. to the existing neurons, in the adult brain. Therefore, problems in the structure and function of the microglia will interfere with the creation of new neurons and their function in the neural network and may lead to mental illnesses such as depression and neurological diseases such as Alzheimer's.
Prof. Yeremia and his team wanted to examine whether changes in the structure and function of the microglia lead to depression and the involvement of these cells in the mechanism of action of anti-depressant therapy (electric shock). To this end, they created a depression-like state in the mice - and exposed them to uncontrollable and unexpected stress stimuli, such as tilting the cage at 45 degrees, flashing light, radio noise, lighting throughout the night and the smell of a predator (rats). Each such stimulus lasted from a few minutes to an hour or two and appeared every day at random for five weeks. The researchers then saw that the mice lost interest and pleasure in activities that should cause this, such as drinking sweet solutions, social play, courtship and sexual behavior, and that they developed despair. These mice were compared to mice that were not exposed to the continuous stress stimuli (control group) which continued to enjoy and participate in these activities.
Chronic stress caused changes in microglia that led to depression
The researchers examined the brains of the experimental mice, and found that the structure and function of the microglia changed dramatically - in the first days of exposure, they were more active, and after a few weeks they shrank and atrophied or even died and disappeared. That is, it was found that continuous stress caused changes in microglia that led to depression.
In another experiment, the researchers sought to prove that the changes in microglia due to the continuous stress are the cause of the development of depression. To this end, the depressed mice were injected with substances that stimulate the immune system that are now used to cure cancer, and it was found in the behavioral tests that they contributed to the disappearance of the symptoms of depression (the mice returned to participate in the activities and enjoyed them despite the stress stimuli). At the end, it was found that the substances did restore the microglia and restored their function - they were able to produce new neurons. That is, a potential antidepressant treatment has been discovered.
Following these findings, the researchers wanted to check whether electric shock - the most effective treatment for severe depression, the underlying mechanism of which is still unclear - affects the microglia. To this end, depressed mice were studied - some were given an electric shock (the experimental group) and some were not (the control group). In the behavioral tests it was found that the treatment did reduce the symptoms of depression (they participated in the activities and enjoyed them). Examining their brains revealed that the structure of the microglia was restored and that the number of newly formed neurons increased. In another group of mice, in which the effect of the electric shock on the microglia was prevented (by injecting a substance that prevents changes in them) - the depression did not go away and the number of new neurons did not increase.
Following this, the researchers wanted to check what is the mechanism in the electric shock that restores the microglia. To this end, we examined with genetic methods (RNA sequencing) which genes change in response to it. It was found that in depressed mice exposed to continuous stress and not treated with an electric shock, the level of the LAG3 gene in microglia increased, while in mice exposed to continuous stress and treated with an electric shock, it decreased and was normal. This gene is part of a control system of the immune system, which regulates its activity. When its level rises - the function of the microglia is damaged. To test the involvement of LAG3 in the antidepressant effect, a group of depressed mice was injected with an antibody that blocks the activity of LAG3 and another group was injected with the antidepressant ciprofloxacin. It was found that the antibody restored the structure of the microglia, increased the production of new neurons and removed the symptoms of depression better than ciprofloxacin. Prof. Yeremia: "We found that this antibody may also be the basis for anti-depressant drugs, and that it may even replace the treatment with electric shock, which is effective against depression, but may damage memory and other cognitive functions."
Life itself:
Prof. Raz Yeremia, 65 years old, married to Nurit, professor of psychology and former chief scientist of the Ministry of Innovation, Science and Technology, and father of four ("Very proud of them: the daughter, a doctor of clinical child psychology, and the sons: a doctoral student in Hebrew literature, a doctoral student in computational biology , and graduated with a master's degree in security studies"). In his spare time he plays the piano and often travels the world.
