For many years viruses that attack bacteria were ignored by the mainstream of researchers, but they have a role in modern medicine, says Vincent Fischetti
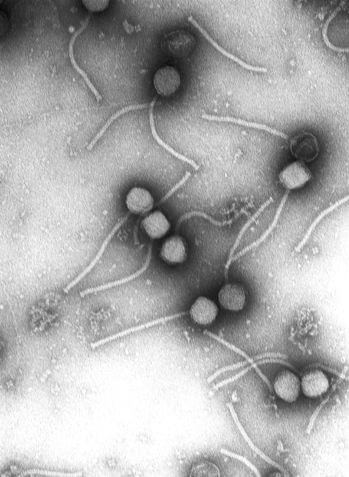
In the laboratory of ContraFect, a small biotechnology company, located on the third floor of a building a few blocks from the Hudson River in Yonkers, New York, they are preparing to test a new and unusual way to kill bacteria in humans. After many years of excessive use of antibiotics, it has lost its sting in the war against the rapid development of bacteria. Today, all the causes of diseases, starting with staphylococcal infections and ending with tuberculosis, have become more deadly and more difficult to treat. The traditional antibiotics are produced from substances secreted by soil bacteria or fungi. Countereffect found an alternative to these substances: bacteriophages, viruses that attack bacteria and take over their internal mechanisms. In nature, phages produce enzymes called lysins, which break down the bacterial cell wall, "explode" them into pieces and allow the hundreds of phages created inside them to be released. At Countereffect, it is believed that they will be able to harness these enzymes to treat infections in humans.
The first clinical trials to test patient safety are scheduled to begin in 2012. And 71-year-old Vincent Fischetti, a microbiologist at Rockefeller University, has been waiting for this moment for decades. As the son of working-class parents, he thought he would be a dentist, but during his undergraduate studies, he became "addicted" to microbiology. He studied for a master's degree in the evenings and during the day financed his studies by working as a technician in a project that dealt with typhoid fever. Meanwhile, he was captivated by the magic of the phages. In 2001, after years of work, he showed that the enzymes from the parenchymal joints help mice fight throat infections caused by streptococcus infection. The US military also sees the inherent potential of these decomposing enzymes in preventing infections when preparing for surgery and cleaning areas contaminated by an anthrax attack by applying them in an ointment.
In general, researchers are showing renewed interest in using mixtures of phages to treat problematic infections. This strategy was practiced in the former Soviet Union, but was completely ignored outside of it. But some technical and practical challenges stand in the way of adopting the strategy for widespread use in human treatment, although several American companies have received approval from the US Food and Drug Administration (FDA) to include phages that kill Escherichia coli and salmonella bacteria in packages of meat and other food products.
A Scientific American reporter spoke with Fishti to learn about the promises and dangers of using phages for human health.
Scientific American: How did you become interested in science?
Fischetti: I grew up on Long Island and my parents had a landscape architecture business right by a lake. Around the age of 12, my parents bought me a microscope. There was no internet back then or anything else that could distract me, so I used to take samples from the lake and spend entire evenings observing the tiny world that I discovered in the water samples: eels, sandals and other kinds of creatures. That's how I occupied myself for hours. And when I took the first course in microbiology at Wagner College in Staten Island, I realized that this is really what I like to do and I stayed in the field.
When did you first become aware of phages?
In my first job I was a laboratory technician at Rockefeller and I worked with John Zabritsky, a physician-scientist. In those days, scientists at New York University discovered that the pertussis toxin - the toxin that causes a whooping cough - is produced by a bacteriophage found in bacteria. We wondered if the toxin that causes anthrax is also controlled by bacteriophage. Indeed this is what we found. Streptococcus bacteria are carriers of a bacteriophage that has a gene for the production of the second toxin. When the bacteriophage multiplies inside the streptococcus, it produces the toxin that causes the redness of the skin and the high fever characteristic of the disease. We now know that bacteriophages are responsible for most toxin-related diseases.
What is the importance of phages to the environment?
In every gram of soil, in every cubic centimeter of water, there are at least 100-10 million phages. Phages are the most numerous creatures on earth. They are everywhere: in food, in drinks, everywhere we touch. We eat and digest fads all the time. They are found in our intestines and mucous membranes everywhere in the body. They infect bacteria and kill them continuously. The resistant bacteria multiply again and the process continues. Every two days, bacteriophages kill half of the bacteria on the surface of the earth. This is a highly dynamic process in which both the bacteria and the bacteriophages need each other to survive. My view is, and I don't know if anyone else thinks like me, that since the number of phages is an order of magnitude greater than that of bacteria, the ones who really rule the earth are the bacteriophages. They control everything.
When did scientists realize that phages could be used in medicine?
100 years ago, when phages were first identified, antibiotics had not yet been discovered, and the feeling was that we had a substance in our hands that we could harness to our advantage to kill infection-causing bacteria. The Pfizer company in the United States was the first to develop phages for medical purposes, and had a plant in Brooklyn for growing bacteriophages to treat infections. But shortly after the company started operating, antibiotics were discovered, and in the US they abandoned the use of bacteriophages to treat infections and chose antibiotics.
And the Soviet scientists chose the other way?
indeed. In several institutions, including one in Tbilisi, Georgia, there are still active bacteriophage treatment programs. People with infections, mainly diabetic foot ulcers that are not cured with antibiotics, come there and are treated with mixtures of bacteriophages. It works, but it's a personal tailoring treatment. Unlike antibiotics, which work against a wide range of bacteria, bacteriophages are unique in that each type of phage only kills a specific bacteria. Essentially, when a person arrives in Tbilisi, they culture the bacteria in the leg ulcer, develop phages that target exactly those bacteria, and the treatment lasts for several weeks. Randall Walcott of the Southwest Regional Center in Lubbock, Texas, also uses bacteriophages to treat resistant bacteria found in contaminated wounds.
Is it the increase in resistance to antibiotics that contributed to the renewal of interest in the use of phages for treatments?
Yes. Antibiotic resistance is a serious problem that entails two issues. One, the bacteria become resistant even to new generation antibiotics. Two types of bacteria are currently the most pressing problem: methicillin-resistant Staphylococcus aureus (MRSA)) and vancomycin-resistant Staphylococcus. In the meantime, they pose a problem for those undergoing surgery who have a weakened immune system, but it won't be long before even an ordinary person who enters a hospital for some minor procedure may become infected with one of the bacteria and become seriously ill. It is almost impossible to treat such an infection, and it is gaining ground not only in hospitals but also in the community.
The other issue is that big pharmaceutical companies are no longer involved in antibiotic development. It is too expensive to invest in the development of a drug that the causes of the disease will be resistant to within a short period of time. This is a very painful problem because these companies are best equipped to develop antibiotic drugs, and I think it is their duty.
What are the obstacles on the way to treatment using phages?
First, the success in Russia (and the former Soviet Union) has not been properly documented. When two individuals suffered the same type of wounds, they were not necessarily treated with the same phage, so it is difficult to document such success in a true scientific way.
Another problem is the need to handle a mixture of phages to kill one creature. Complex mixtures have difficulty getting approval from the FDA, especially for mixtures of bacteriophages, which naturally absorb bacterial DNA and the FDA would certainly want to know what bacterial DNA they carry. Phage therapy companies are trying to get approval, and it's not to say that it will never be achieved, but they still have a bitter battle ahead of them before they get approval to treat humans.
Are there other ways to utilize the benefits of phages in medicine?
One way we have developed is the use of phage wall-dissolving enzymes. When phages enter a bacterium they enslave the bacterium to create new phage particles. At the end of the process they must break their way out of the bacterium. For this purpose, they produce an enzyme that breaks down the cell wall of the bacterium and thus causes it to explode. We isolated the enzyme and we add it to our target bacteria. The enzyme drills a hole in the cell wall and the bacteria actually dies immediately. In humans, these enzymes can be applied directly to the skin or mucous membranes, or injected into the blood. Since the enzymes are quickly eliminated from the body and cannot break down tissues in humans we expect them to be safe.
How did you come to know that these enzymes can be used for treatment?
40 years ago I isolated an enzyme from such a joint in my doctoral thesis. At the same time, I used it to disassemble the cell wall of the streptococcus bacterium to learn about its surface proteins. But my real medical breakthrough happened ten years ago. I had mice carrying Streptococcus A in their throats. When I applied the decomposing enzyme to their throats it turned out to kill the bacteria immediately. Then I realized that enzymes can be used for treatments. It was a "wow" moment! This was the first time anyone had used the degradative enzyme in an animal model and shown a therapeutic effect.
We have since used these enzymes to treat endocarditis, which damages the heart valves in laboratory animals, and to study meningitis. We also use enzymes to treat pneumonia, group B streptococcus and bacteremia - a blood infection. The enzymes are very stable. They can be frozen or dried for many years and they still retain their activity.
very impressive. Do other scientists see the northern medicinal abilities in these enzymes?
It was hard. People said, "That's interesting, but..." The pharmaceutical industry was worried that the immune system would create antibodies in the body against the enzymes and neutralize them. Also people were bothered by the specificity of the enzymes. The streptococcus enzyme only kills streptococcus, the pneumonia enzyme only kills pneumococcus, and the anthrax enzyme only kills anthrax. They said, “You know, it's too targeted. We need enzymes with a wide range of activity."
Today we have enzymes whose activity is extensive, but such activity is not desirable because this way we also kill good bacteria and create other problems. It is better to kill the creatures we wish to kill without causing harm and without also killing creatures that are necessary for human health and well-being. I think this is the direction everyone is heading: to try to kill what they want to eliminate without destroying anything else in the body.
And are there other ways to use these enzymes to keep the body healthy?
Indeed, there is. We developed an enzyme that kills anthrax. Ten years passed until the government realized that if a terrorist attack were to occur in which anthrax spores were scattered throughout the city, it would take decades to safely remove all the spores from the environment. And in order to do this, you must use nutritious substances. What we were able to do in the laboratory is to add to the enzyme that breaks down the anthrax cell wall a natural substance that deceives the spore and causes it to germinate. Within 20 minutes you can eliminate 99.99% of the spores. The product is soluble in water, very safe and can be used to purify large areas contaminated with spores.
Can a bacterium develop resistance to the disintegrating enzymes?
So far we have not found any bacteria resistant to these enzymes. I think this is due to the billions of years in which the enzymes evolved and focused on those parts of the bacteria that they cannot change. While never say never, developing resistance will be a very rare event.
This year begins the first clinical trial of Contraafect with 301-CF, a decomposing enzyme that you discovered against MRSA. Is this the first experiment with these enzymes done in humans?
exactly. This will be the first time that decomposing enzymes have been used in humans.
I take it you are very excited about the experiment?
very excited It took ten years of hard work to get there.
About the author
Bernard Burrell of New York is a frequent contributor to Scientific American and Nature
For a broader article about this research work (in English):

3 תגובות
The basic idea of using natural weapons in the existential war between phages and bacteria is amazing. With the advanced use of powerful computer systems and artificial intelligence in order to coordinate the destructive efficiency. And that is through bioinformatics. Those who are strong in mathematics are the playing field to make a very profitable and interesting career.. the 8200 of biology..
I don't know how reliable it is, but I read somewhere that the Red Army was able to cure many of its soldiers (who were affected by typhus, dysentery, and others from the Bishin mine) in the bloody battles for the defense of Stalingrad (1942-3) by using a secret preparation, which was probably based on the use of phages produced from sewage water!!!!???
I've read about the nosa a million times and never understood why they don't use it
It is found abundantly in humans and is also considered very safe
And to get them, the director of the institute in Tbilisi said that they go down the drain because that's where the most phages are
Conclusion: square humans