The researchers of the Faculty of Biomedical Engineering at the Technion developed the tissue by printing with biological ink
Researchers at the Faculty of Biomedical Engineering at the Technion have developed Engineered tissues with a branched (hierarchical) network of blood vessels. These tissues are intended for quick and efficient transplantation in damaged organs.
the current research, Published in Advanced Materials, focused on the development of the vascular network around the coronary artery that supplies blood to the heart muscle. The research was conducted by Prof. Shulamit Levenberg, head of the laboratory for tissue engineering and stem cells in the Faculty of Biomedical Engineering at the Technion, and the doctoral student (now Dr.) Ariel Shaklani, with their colleagues from the Technion, the Czech Republic and the USA.
The blood vessels in our body are the oxygen pipe of the living cell, literally, and therefore they are essential for the function of the tissue. Without them the cell does not receive oxygen and nutrients and cannot survive. Therefore, one of the challenges in creating tissues for transplantation is the creation of a flap (FLAP) - a tissue containing blood vessels; If these blood vessels successfully connect to the natural vascular network in the target tissue, they accelerate the absorption of the suspension in the body. Existing approaches focus on the creation of medium vessels for transplantation or branching models of tiny vessels, But the combination between the two is a new achievement of the technical research group.
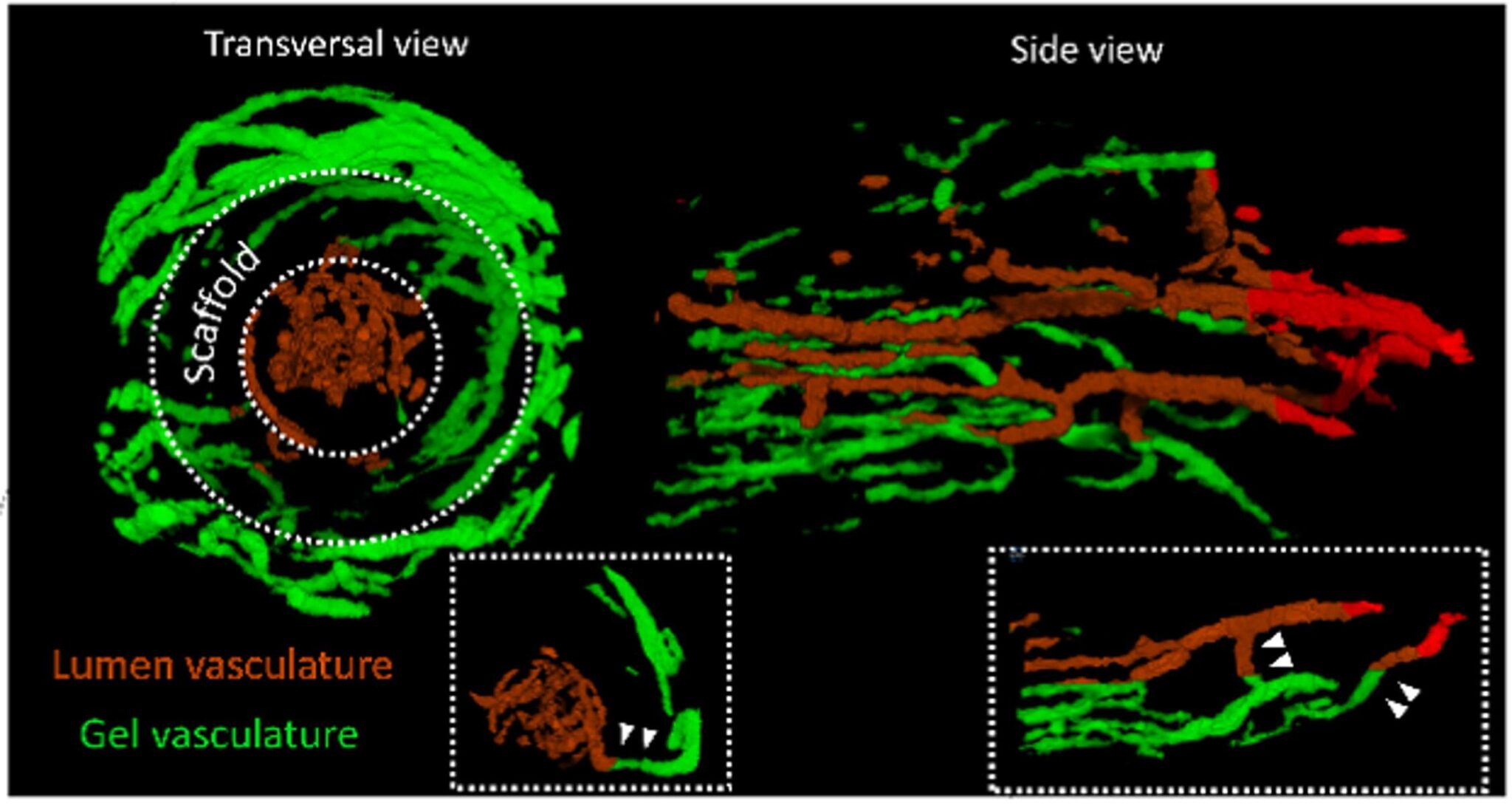
Compared to the first engineered scaffolds, which contained only an artery, more advanced scaffolds contain branched vascular networks in which medium-sized vessels branch off from the main artery and from which small vessels. This network is similar to a tree, that is, thin branches that branch off from larger branches that grow from the trunk of the tree, and more importantly - it imitates the natural blood vessel network.
In recent years, Prof. Levenberg presented several breakthroughs in this context of engineered tissues containing branched networks of blood vessels. The growth of these racks is based on Degradable XNUMXD polymeric scaffolds, on which she grows the tissues in the laboratory. Biological cells (fibroblasts and endothelial cells) essential for the development of blood vessels are seeded on the scaffolds. This is how the research group created complex and relatively efficient racks.
However, to improve the suspension before implanting it in the affected area in the animal is required so far Mid Level where the sling was implanted in a different place from the injury area and moved from there to the injured area after a certain period of time. This period gave the sling essential properties of natural tissue, which improved its absorption in the injured area of the animal. A similar result was obtained in the present study without the need for the temporary transplant. This is partly thanks to the use ofXNUMXD biological printing based on biological ink. The printing method was also developed in Prof. Levenberg's laboratory.
In the current study, the researchers used human collagen grown in tobacco (a development of the CollPlant company) as the biological ink for printing the cells. This is instead of the usual use of collagen extracted from animals.
In the first stage of the development, the researchers printed the hollow main artery and, in the printing process, created small holes in it to encourage blood vessels to spring into the printed tissue that is placed around the main tube. Around the artery and inside it they seeded endothelial cells that encourage the sprouting of blood vessel cells; Indeed, medium and small blood vessels came out of the holes in the artery and thus a branched network system was formed.
To test the effectiveness of the new suspension, they connected it, using the engineered artery, to the femoral artery of a rat. About two weeks after the implantation of the scaffold in the body of the rat, its success was verified by tomography (micro CT) which showed the presence of contrast material injected into the vascular system of the rat within the engineered branching network.
Shaklani and Prof. Levenberg estimate that this work is an important step towards personalized medicine that combines collagen ink, scaffolds produced based on medical imaging and intentionally sorted cells (iPSC) derived from the patient's own cells. According to Prof. Levenberg, "Although the current research focused on the coronary artery and the environment of the heart, the new concept is also relevant to the rest of the body's tissues. The next step will be to try to apply the approach in larger animals, this is towards its application in humans."
The research was supported by an ERC grant from the European Research Commission. The Czech Science Foundation supported the visit of a student from the Czech Republic to the Technion to learn tissue engineering methods developed in the Levenberg laboratory.
Dr. Ariel Shaklani who was a partner in the research was born in Buenos Aires, Argentina and studied biomedical engineering at UNER (Universidad Nacional de Entre Ríos). "During the years of study in Argentina, I wanted to enter the field of tissue engineering, and my goal was to do a doctorate with Prof. Levenberg. I wasn't looking anywhere else in the world, and happily it accepted me."
Sheklani immigrated to Israel with his wife in 2014 and together they started studying at the Technion in 2015. Dr. Shaklani is currently a co-founder and CTO of Plantish, a company that develops technology for the production of plant-based salmon substitutes.
for the article in Advanced materials
More of the topic in Hayadan:
- From the heart
- The google maps of the brain: locating RNA fragments in brain cells without removing the tissue
- The organization of the quality control system of proteins affects the onset of neurodegenerative diseases
- Success in creating an engineered implant that replaces damaged bone tissue
- The strange and "noisy" method in which leaves are used to grow
