The technology developed by Prof. Yuval Shaked's research group was registered as a patent and is now in the process of being commercialized
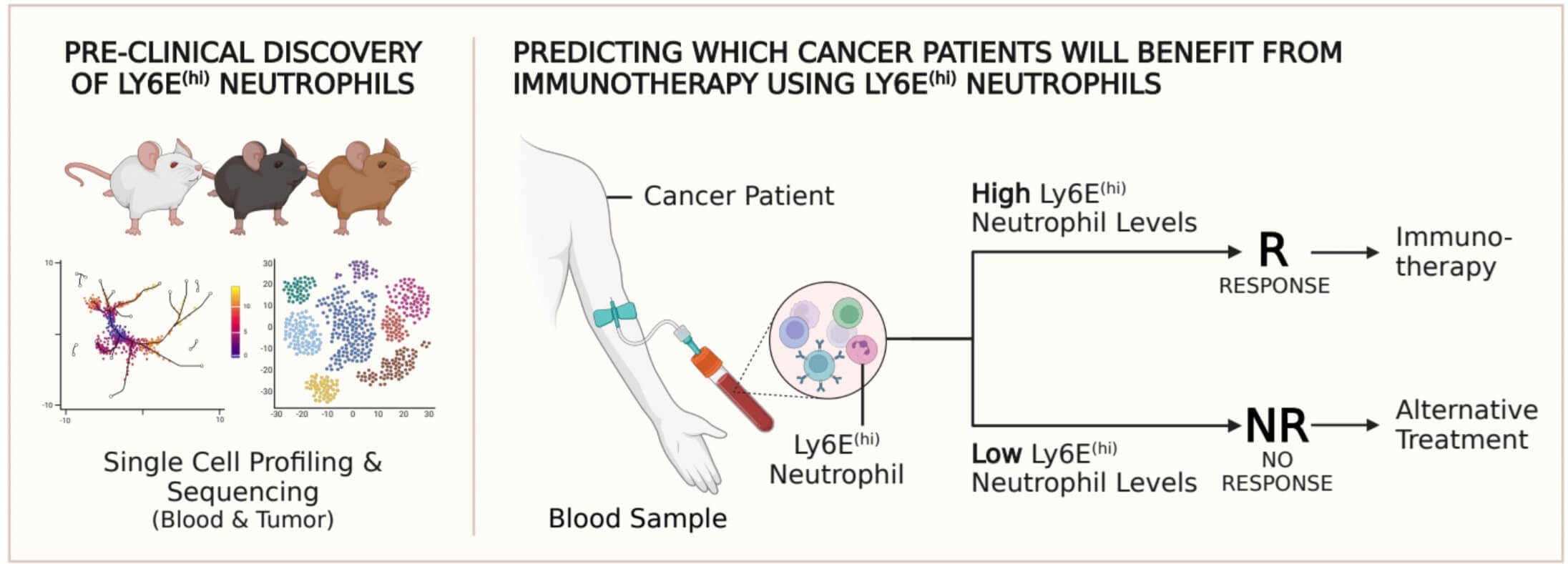
Researchers at the Rappaport Faculty of Medicine at the Technion have discovered new blood cells that predict the success of immunotherapy. The findings are expected to optimize the adaptation of the treatment to the specific patient, and their importance stems from the fact that it is very important to identify in advance the patients who respond to the treatment. the research published in the prestigious journal Cancer Cell Led, with an equal contribution to the research and the article, Dr. Madeleine Ben Gigi and the post-doctoral student Dr. Tim Cooper under the guidance of Prof. Yuval Shaked from the Rapaport Faculty of Medicine. This is translational research based on RNA sequencing (scRNA-seq), analysis of existing information, preclinical models of cancer and confirmation of the findings in humans.
immunotherapy Considered one of the biggest revolutions in cancer treatment. It is based on the understanding that the natural immune system excels at attacking cancer cells selectively and accurately. The problem is that in many cases, the cancerous tumor deceives her and prevents her from recognizing it as an enemy and thus escapes her. In such a case, immunotherapy holds that, instead of attacking the cancer with chemotherapy drugs that also damage the healthy tissues, it is better help the immune system Identifying the cancer cells as the enemy and letting it do the rest of the work itself.
Despite the dizzying success of the immunotherapy approach in cancer treatment, its effectiveness is still very limited to about 40% of patients. This means that many patients receive this harsh treatment without positive results. Hence the important need for a thorough understanding of biological responses to such treatments and for detection Biomarkers which predict well the future success of the treatment. Biomarkers are an important element in the era of personalized medicine. They make it possible to make informed medical decisions and formulate an optimal treatment plan adapted to the specific patient and his medical profile.
Today, biological markers are already used in immunotherapy treatments, but these are taken by biopsy - a process that may endanger the patient. In addition, this approach does not sufficiently consider the immune profile of the patientspecific And her predictability is lacking, to say the least. For this reason, many studies in the field, both in industry and in academia, strive to find new ways to predict which patients will respond to immunotherapy.
And hence - to the research itself
The Technion researchers, who focused on antibody-based immunotherapy, discovered Biomarkers that predict the specific patient's response to treatment. Since these markers are found in the blood, they do not require taking a biopsy from the tumor - an invasive process that is sometimes not applicable and, as mentioned, sometimes puts the patient at risk.
Schematically, the mechanism discovered by the researchers is this: a protein called STING, which activates the immune system, comes into action in the face of cancer development, and is more pronounced mainly in cancer cells that will respond to the immunotherapy treatment. This protein results in the expression of an interferon protein which in turn stimulates neutrophils to differentiate into a specific type (which expresses the Ly6E proteinhi). These neutrophils act directly on the immune system and stimulate it against the cancer tumor. Therefore, the researchers concluded that testing Ly6E neutrophil levelshi The patient's blood can be used as an effective biomarker in predicting the response to the immunotherapy treatment. The researchers examined these findings, which were based on preclinical research, on cancer patients (lungs and melanoma), while cross-checking with existing records, and demonstrated the ability of the neutrophils To predict the response of patients to immunotherapy with high accuracy also in humans.
The researchers discovered that beyond their value as important biological markers, The neutrophils may also aid in the treatment itself. The presence of these neurophils in the tumor creates a higher sensitivity to the immunotherapy treatment. These findings are consistent with an analysis of existing data on 1,237 cancer patients who underwent antibody-based immunotherapy treatments. The researchers found that
In most of the samples from those patients, a relationship was found between the levels of neutrophils and the patient's response to immunotherapy.
The technology developed by Prof. Yuval Shaked's research group was registered as a patent and is now in the process of commercialization (tech transfer) with OncoHost for further development. Prof. Shaked points out that the technology can be used in the common FACS machine, which is found in almost every hospital and approved by the regulatory authorities.
Various research groups in Israel and around the world participated in the study, including doctors and researchers from Hadassah, Rambam, Sheba, Haifa University, Heidelberg University (Germany) and Yale University (United States).
The research was supported by the European Research Commission (ERC grant), the National Science Foundation, the American Institutes of Health (NIH), the Ariane de Rothschild Foundation (Ariane de Rothschild scholarship for outstanding doctoral students) and the RTICC-Rubinstein scholarship on behalf of the Baruch and Ruth Rappaport Center for Integrated Cancer Research at the Technion.
More of the topic in Hayadan:
- A new study sheds light on an important mechanism in the degradation of white blood cells
- Towards personalized treatment of melanoma skin cancer
- The chances of success of immunotherapy depend on the degree of heterogeneity of the cancer tumor
- Weizmann Institute scientists have developed a method for calculating differences between different odorants
- How to prevent the body from helping cancer instead of fighting it
