American grant to researchers from the Technion and Johns Hopkins University
Researchers from the Technion and Johns Hopkins University received a competitive grant for the development of an innovative technology that will assist in the treatment of juvenile diabetes patients. The prestigious grant, 700 thousand dollars on behalf of JDRF (World Youth Diabetes Research Fund), will be awarded to Dr. Shadi Farah from the Wolfson Faculty of Chemical Engineering at the Technion and his colleague from Johns Hopkins University Dr. Joshua Dolloff.
Juvenile diabetes, or type 1 diabetes, is an autoimmune disease, meaning a disease caused by an attack of the immune system on the body's cells. This attack leads to the destruction of pancreatic cells - cells that produce insulin - and subsequently to severe damage to various tissues.
Insulin is an essential hormone involved in many biological processes, including tissue creation, energy storage, blood glucose regulation and slowing down the breakdown of protein and fat tissues. The lack of insulin in the bodies of juvenile diabetics leads, among other things, to the breakdown of vital tissues, the accumulation of glucose and damage to blood vessels - damage that can cause damage to the kidneys, eyes and other organs.
The common treatment for juvenile diabetes is a daily injection of insulin to the patient. Due to the discomfort that characterizes this treatment, various devices have been developed in recent decades that provide the body with insulin without the need for daily treatment. These devices, which contain insulin-producing pancreatic islets, are implanted in the patient's body and release insulin at the required rate.
The problem is that like the pancreatic cells of the diabetics, too The devices themselves are attacked by the immune system which treats them as a foreign body. Since the body cannot remove the device from it, it "suffocates" it within thick walls of scar tissue. These walls block the entry of oxygen, sugar and other essential substances to the pancreatic islets and cause their death.
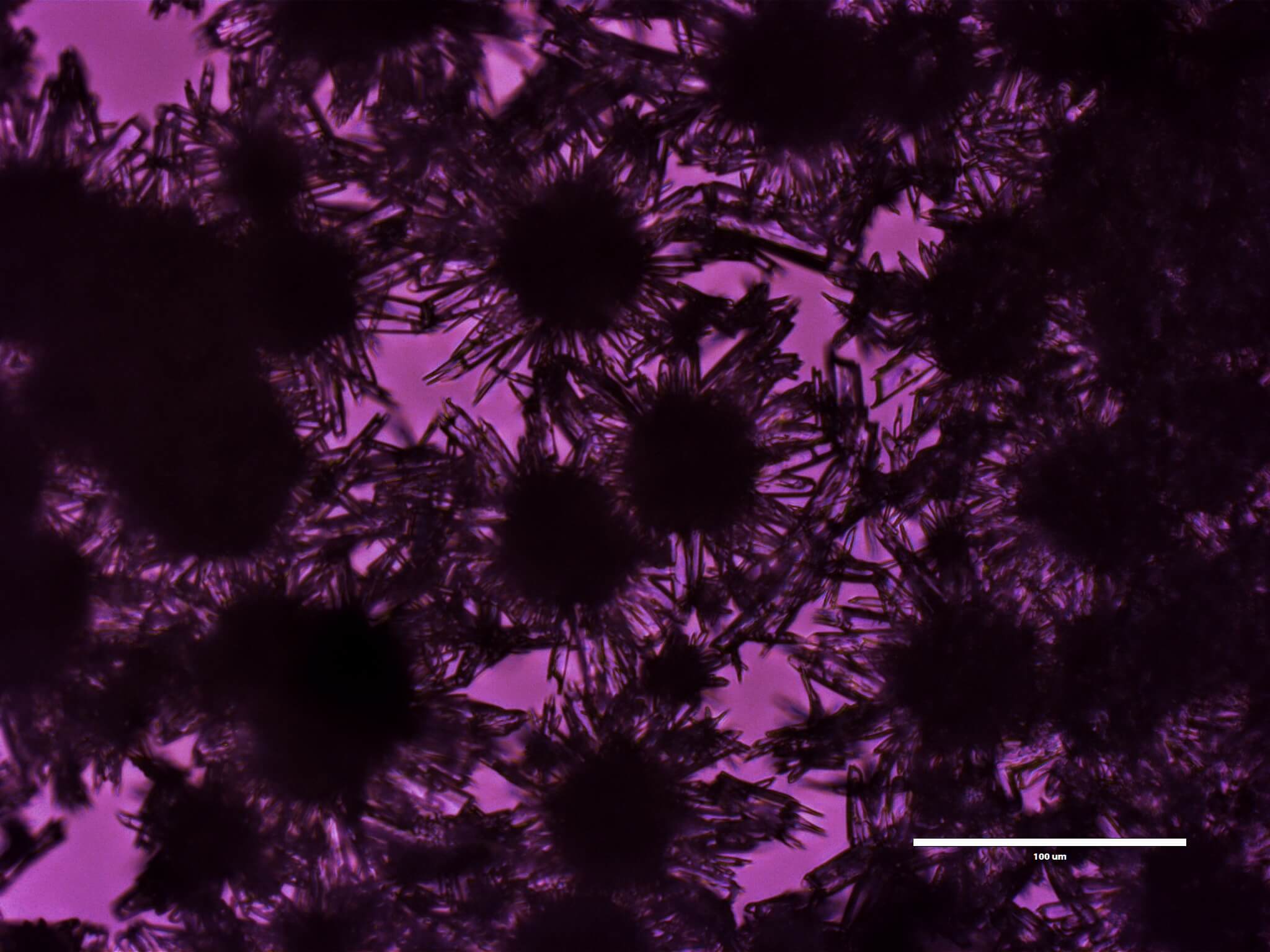
Dr. Farah and Dr. Doloff developed a crystalline transport platform that releases an anti-inflammatory drug inside the device and thus supports the survival of the pancreatic islets. This platform allows slow release of the drug for months and even years without the need for carriers to control the release rate. Based on the grant, they will test the platform and improve it for clinical use.
More of the topic in Hayadan:
